Take a Warm Bath 1 to 2 Hours Before Bedtime to Get Better Sleep, Researchers Find
Bath time isn't just for fun and relaxation—researchers have now discovered that climbing into the tub before bed can help you get a better night's sleep.
Scientists are quickly discovering that our gut microbiomes may hold the key to a vast amount of health issues-including ALS.
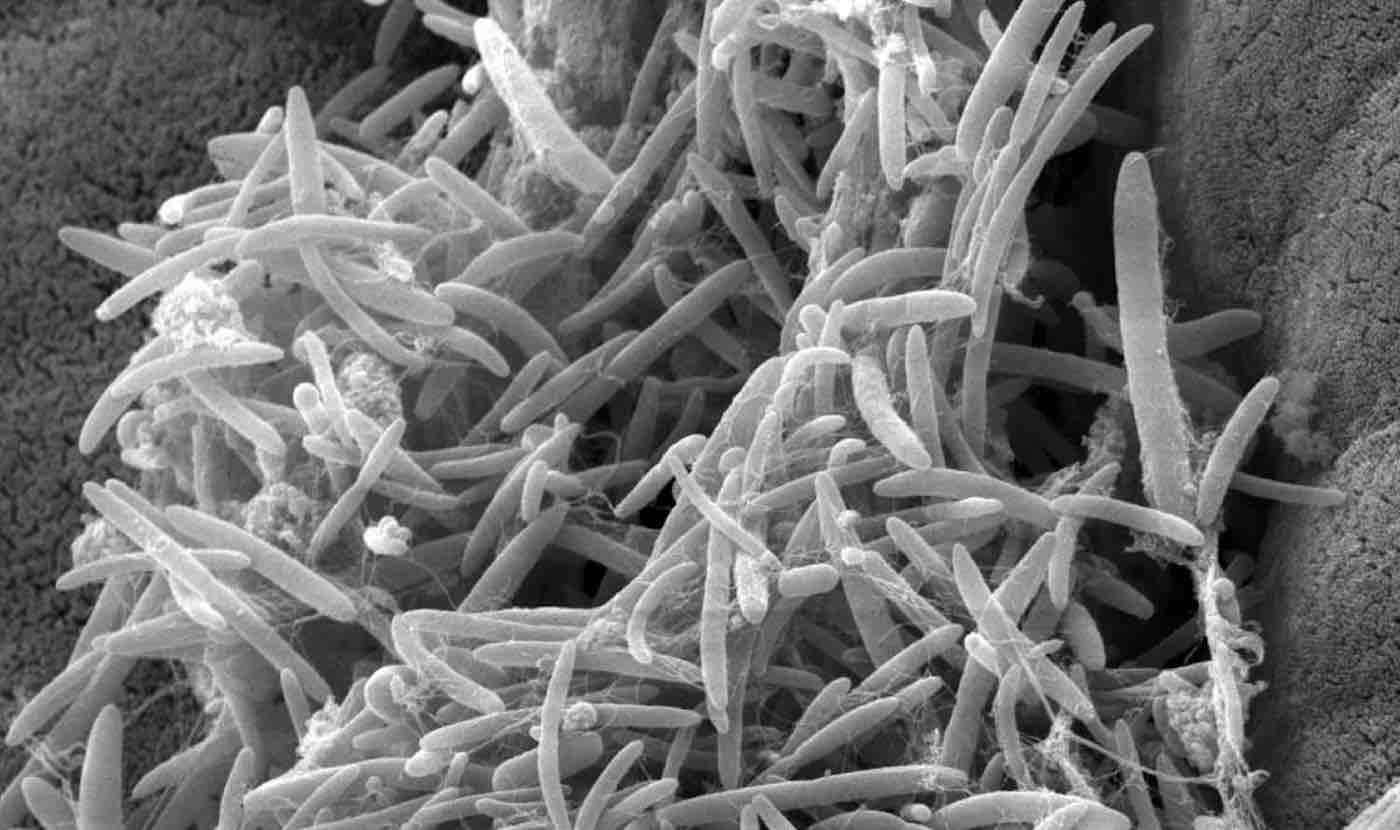
Researchers at the Weizmann Institute of Science have shown in mice that intestinal microbes, collectively termed the gut microbiome, may affect the course of amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig's disease.
As reported this week in Nature, progression of an ALS-like disease was slowed after the mice received certain strains of gut microbes or substances known to be secreted by these microbes-and results suggest that these findings are likely applicable to human patients with ALS.
"Our long-standing scientific and medical goal is to elucidate the impact of the microbiome on human health and disease, with the brain being a fascinating new frontier," says Professor Eran Elinav of the Immunology Department.
The scientists started out demonstrating in a series of experiments that the symptoms of an ALS-like disease in transgenic mice worsened after these mice were given broad-spectrum antibiotics to wipe out a substantial portion of their microbiome. Additionally, the scientists found that growing these ALS-prone mice in germ-free conditions (in which, by definition, mice carry no microbiome of their own), is exceedingly difficult, as these mice had a hard time surviving in the sterile environment. Together, these results hinted at a potential link between alterations in the microbiome and accelerated disease progression in mice that were genetically susceptible to ALS.
Next, using advanced computational methods, the scientists characterized the composition and function of the microbiome in the ALS-prone mice, comparing them to regular mice. They identified 11 microbial strains that became altered in ALS-prone mice as the disease progressed or even before the mice developed overt ALS symptoms. When the scientists isolated these microbial strains and gave them one by one-in the form of probiotic-like supplements-to ALS-prone mice following antibiotic treatment, some of these strains had a clear negative impact on the ALS-like disease. But one strain, Akkermansia muciniphila, significantly slowed disease progression in the mice and prolonged their survival.
To reveal the mechanism by which Akkermansia may be producing its effect, the scientists examined thousands of small molecules secreted by the gut microbes. They zeroed in on one molecule called nicotinamide (NAM): Its levels in the blood and in the cerebrospinal fluid of ALS-prone mice were reduced following antibiotic treatment and increased after these mice were supplemented with Akkermansia, which was able to secrete this molecule.
To confirm that NAM was indeed a microbiome-secreted molecule that could hinder the course of ALS, the scientists continuously infused the ALS-prone mice with NAM. The clinical condition of these mice improved significantly. A detailed study of gene expression in their brains suggested that NAM improved the functioning of their motor neurons.
Finally, the researchers examined the microbiome and metabolite profiles of 37 human ALS patients and compared them to those of family members sharing the same household. A detailed genomic analysis suggested that the gut microbiomes of ALS patients were distinct in composition and functional features from those of healthy controls. In particular, numerous microbial genes involved in the synthesis of NAM were significantly suppressed in ALS patients.
An analysis of thousands of small molecules in the blood also revealed a distinct pattern in ALS patients as compared to controls. Here too, many of the intermediary molecules involved in the NAM synthesis were altered in the blood of ALS patients. When the researchers tested the levels of NAM itself, they found these to be significantly reduced in both the blood and the brain of 60 human ALS patients as compared to controls. Moreover, there was a correlation between reduced NAM levels and the degree of muscle weakness in the patients.
"These findings are only a first step towards achieving a comprehensive understanding of the potential impact of the microbiome on ALS," Elinav says, "but they suggest that in the future, various means of altering the microbiome may be harnessed for developing new therapeutic options for ALS."
Reprinted from the Weizmann Institute of Science
Treat Your Friends For Negativity By Sharing The Exciting Breakthrough To Social Media…
Be the first to comment